With chronic pain affecting over 58 million American adults—a number projected to reach 78 million by 2040—the search for effective, non-invasive pain management solutions has never been more urgent. Pulsed Electromagnetic Field (PEMF) therapy has emerged as a promising complementary treatment, but understanding how it actually works at the cellular level can help you determine if it’s right for your pain management strategy.
What Makes PEMF Different from Other Pain Therapies?
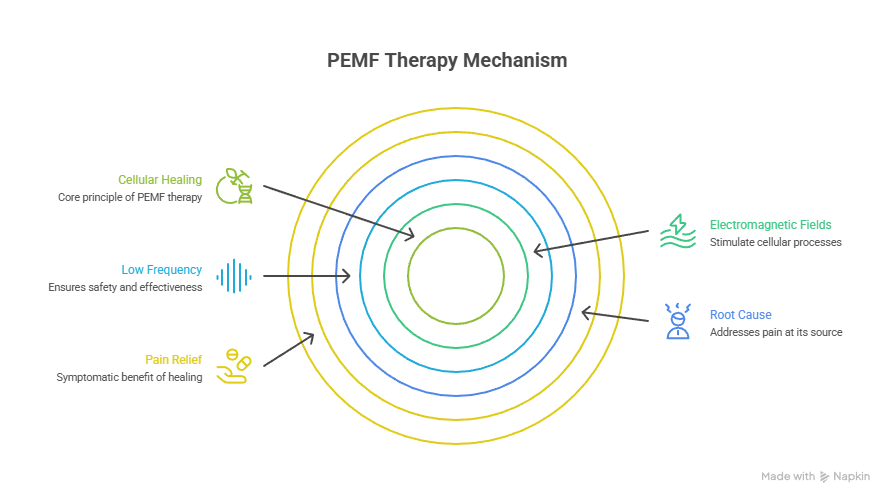
Unlike pain medications that mask symptoms or TENS units that simply block pain signals to the brain, PEMF therapy operates on a fundamentally different principle. It penetrates deep into tissues to address the root cause of pain at the cellular level.
PEMF therapy uses low-frequency electromagnetic fields—typically 1000 Hz or less—to stimulate cellular repair and regeneration. These are subthreshold, low-power electromagnetic waveforms specifically designed to target cells without causing thermal effects or tissue damage. The key difference? PEMF doesn’t just interrupt pain signals; it actively promotes healing by recharging depleted cells and triggering natural repair mechanisms.
The Cellular Energy Connection: How PEMF Actually Works
Your body’s cells function like tiny batteries, and chronic pain often indicates that these batteries are running low. Stress, injury, inflammation, and disease all deplete cellular energy, slowing down the healing process and perpetuating pain cycles.
PEMF therapy addresses this at the most fundamental level by increasing ATP (adenosine triphosphate) production—the energy currency your cells use to function. When electromagnetic pulses penetrate your tissues, they restore the electrical potential of damaged cells, essentially “recharging” them. This energy boost kickstarts repair processes that may have stalled due to injury or chronic inflammation.
The Bioelectromagnetic Principle: All cells function and communicate based on principles of bioelectromagnetics. PEMF therapy works because it modulates cell functions and enhances energy levels through improved oxygen capacity, leading to genuine long-term healing rather than temporary symptom relief.
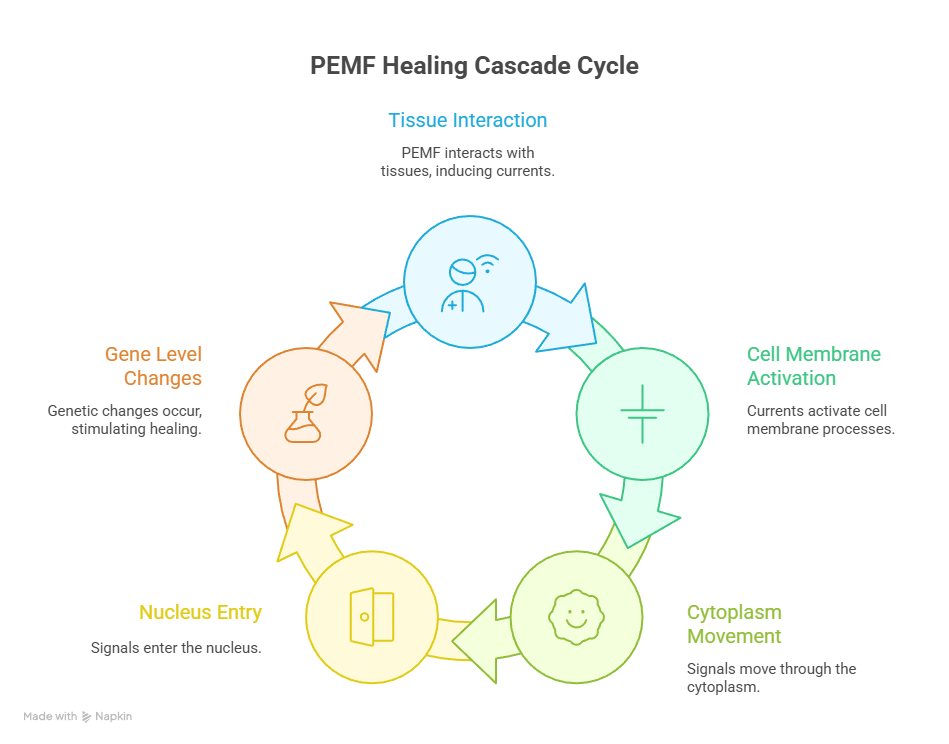
From Cell Membrane to Gene Level: The Healing Cascade
The healing effects of PEMF aren’t superficial. When electromagnetic pulses interact with your tissues, they initiate a sophisticated cascade of biological activities that flow from the cell membrane all the way to the gene level.
Here’s what happens: The currents induced in tissues by PEMF mimic the natural electrical activities created within bones during movement. These pulsing magnetic fields trigger a sequence of events—starting at the cell membrane, moving through the cytoplasm to the nucleus, and ultimately reaching the genetic level where specific changes take place. This is why PEMF can stimulate the osteogenic activity of osteoblasts (bone-building cells) and promote actual tissue remodeling, not just temporary pain relief.
Why Low-Intensity Fields Work Better
It might seem counterintuitive, but PEMF’s gentle approach is precisely what makes it effective. The therapy uses electromagnetic fields of remarkably low strength—approximately 200 μT at the head surface to 35 μT deep in the brain for cranial applications, and similar low levels for joint and tissue treatments.
Unlike more aggressive treatments that can cause collateral damage, these low-intensity fields trigger gentle tissue repair while leaving healthy cells undisturbed. The anti-inflammatory and anti-edema effects of PEMF appear in all compartments of injured tissue simultaneously, rather than depending on pharmacokinetics like medications do. This means PEMF works consistently throughout the treatment area, regardless of blood flow or absorption issues that can limit drug effectiveness.
Tissue-Specific Applications: Not All Pain Is Created Equal
One of PEMF’s most valuable characteristics is its adaptability to different tissue types and pain conditions. The therapy has demonstrated efficacy across a spectrum of chronic pain syndromes (for athletes specifically, check out our complete protocol guide for athletic recovery):
- Osteoarthritis: PEMF stimulates cells that maintain and repair cartilage while reducing the inflammatory environment contributing to joint degradation. Studies show significant pain reduction and improved physical function in OA patients.
- Rheumatoid Arthritis: For this autoimmune condition, PEMF helps moderate inflammatory responses and regulate the overactive immune response, potentially decreasing the frequency and severity of flare-ups.
- Fibromyalgia: Research indicates a differential effect of PEMF in fibromyalgia patients, with notable improvements in pain levels and quality of life—suggesting PEMF may be particularly effective for conditions with presumed central pain mechanisms.
- Post-Surgical Recovery: PEMF excels in post-surgical joint recovery by promoting faster bone integration with prosthetic components, reducing post-operative swelling, and enabling patients to begin rehabilitation sooner.
- Chronic Low Back Pain: Systematic reviews suggest PEMF is beneficial for non-specific low back pain, particularly when used as an addition to conventional physical therapy modalities.
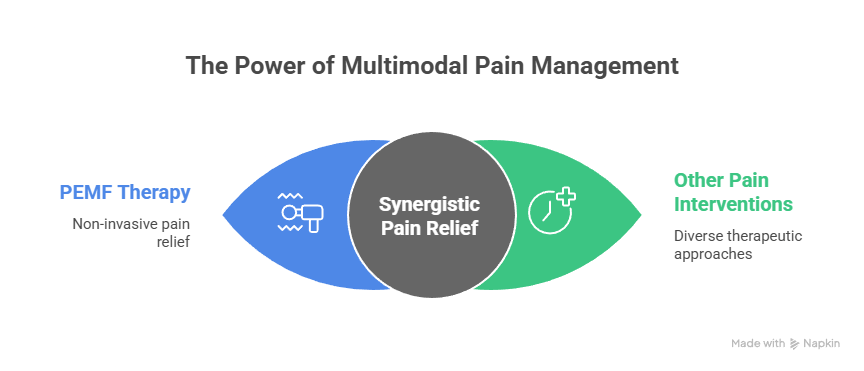
Building Your Multimodal Pain Management Strategy
The future of pain management lies in multimodal approaches—combining different therapies to achieve cumulative and synergistic effects. PEMF fits perfectly into this framework as a complementary treatment that can enhance other interventions.
Here’s how to think about integration:
- With Physical Therapy: PEMF can be used before physical therapy sessions to reduce inflammation and pain, making exercises more tolerable and effective. The combination shows better outcomes than either treatment alone.
- Medication Reduction: PEMF improves pain relief by allowing lower medication amounts, thus minimizing side effects. This is particularly valuable for patients concerned about long-term NSAID use or seeking to reduce opioid dependence.
- Post-Procedure Adjunct: PEMFs can be applied after arthroscopic knee procedures or joint replacements to control post-operative inflammation and pain, potentially accelerating recovery timelines.
The goal is customization—tailoring your multimodal analgesia according to your specific needs, condition severity, and response to treatment.
What to Expect: Treatment Protocols and Timelines
Understanding realistic expectations helps you commit to a treatment protocol and evaluate its effectiveness. Most clinical studies use the following parameters:
- Session Duration: 30-60 minutes per session
- Frequency: 2-3 sessions per week
- Initial Protocol: 4-6 weeks for the first treatment phase
- Sensation: Most patients describe a gentle pulsing or warming feeling during treatment
For acute conditions or post-surgical applications, you may need more frequent sessions initially. Chronic conditions typically benefit from consistent, sustained treatment over several weeks, with maintenance sessions as needed. The key is patience—PEMF promotes actual healing and tissue remodeling, which takes time compared to medications that provide immediate but temporary relief.
Navigating Device Selection and Safety
PEMF devices vary considerably in design and application methods. Understanding these differences helps you make informed decisions (for a detailed review of one popular portable option, see our science-backed analysis of the Vibe PEMF device):
Device Types: PEMF systems typically include either full-body mats for generalized exposure or targeted applicators (belts, pads, or localized devices) for specific problem areas. Some advanced systems offer both options for flexibility.
FDA Clearance: Look for FDA-cleared devices that emit electromagnetic pulses at specific frequencies shown to promote healing. This clearance indicates the device has met safety and efficacy standards for its intended use.
Safety Profile: PEMF has been shown to be a safe therapy with minimal side effects. The therapy has been studied for over 30 years with no concrete evidence of harm when used appropriately. However, PEMF may not be suitable for individuals with pacemakers, insulin pumps, or during pregnancy—always consult your healthcare provider before beginning treatment.
The Evidence: What Research Actually Shows
While testimonials abound, it’s important to ground expectations in actual research. The evidence base for PEMF includes:
- Systematic reviews demonstrating pain reduction and functional improvement in osteoarthritis management
- Randomized controlled trials showing efficacy for chronic low back pain, particularly as an adjunct to conventional therapy
- Clinical studies documenting reduced inflammation and accelerated bone healing
- Case reports of significant relief in conditions like interstitial cystitis/bladder pain syndrome
However, researchers note that further high-quality studies with larger sample sizes and standardized protocols are necessary. Studies should also focus on determining the optimal parameters of frequency and intensity for different pain conditions. This ongoing research will help refine PEMF applications and identify which patients benefit most.
The Bottom Line: PEMF therapy represents a valid, evidence-supported option for pain management that works through genuine biological mechanisms rather than placebo effects. While not a miracle cure, it offers a safe, non-invasive way to support your body’s natural healing processes and potentially reduce dependence on medications.
Ready to Explore PEMF Therapy?
If you’re dealing with chronic pain and seeking complementary treatment options, consider discussing PEMF therapy with your healthcare provider. They can help determine if it’s appropriate for your specific condition and guide you toward reputable treatment options or FDA-cleared devices.